“It ain’t what you don’t know that gets you in trouble; it’s what you know that just ain’t so.”
Samuel Clemens
I am going to make some generalizations here. As with all generalizations, there are exceptions, but I believe my premise holds true enough to be valid.
The trajectory of medicine seems hellbent on lowering medical care to the lowest common denominator. More and more medical “professionals” are entering the arena, claiming enough education and experience to provide treatment independent of physicians. These include nurse practitioners, physician’s assistants, pharmacists, optometrists, and will doubtless include evermore para-medical professionals. Think EMTs, massage therapists, etc. This doesn’t even include such fringe practitioners who already promote themselves as alternatives to physicians, e.g. homeopaths, acupuncturists, reflexologists, Frankhauser manipulators, and a veritable army of “alternative” medicine providers. Every legislative session in state and federal government seems to include one or more bills related directly to expanding the “scope of practice” of a non-physician group.
One example of this is the expansion of vaccinations to pharmacies. Pharmacists do not receive any training in direct patient care. They don’t learn how to treat patients or manage complications of treatment. They go through a training program that involves self-study and learning the mechanics of performing an injection. You can train anyone to give injections; children with diabetes learn to give themselves insulin shots. The problem is that once you give pharmacists license to evaluate patients and autonomously dispense vaccines, it is a pretty short hop to evaluating patients and writing prescriptions themselves. Pharmacists have worked well with physicians for generations. Seeking autonomy now, makes little sense.
A recent experience was telling. I had to get the diptheria/tetanus/pertusis (DTaP) vaccine for the impending arrival of my newest granddaughter. For expediency, and out of curiosity, I went to my local Walgreens for this. After a short wait, I was ushered into a small room with a young pharmacist who was clearly nervous. No history was taken, no inquiry as to allergies, no blood pressure or vital signs. When he performed the injection, he expressed surprise that so little material was injected and examined the syringe for, I suppose, any defects. The vaccine volume was 0.5 cc, a minute amount so this was perfectly expected but it clearly surprised him. I walked away with little in the way of increased confidence in this avenue for vaccinations.
Physicians, the most highly educated, trained, and experienced medical professionals are no longer directing medical care. We are being bypassed and disenfranchised largely by legislators, many of whom take positions based, it seems, largely on who has the most effective lobbyists or provides the greatest number of potential voters. The ship of medicine will soon no longer have a captain, only a bunch of sailors, each claiming autonomy to sail on their own. I believe this is a recipe for disaster.
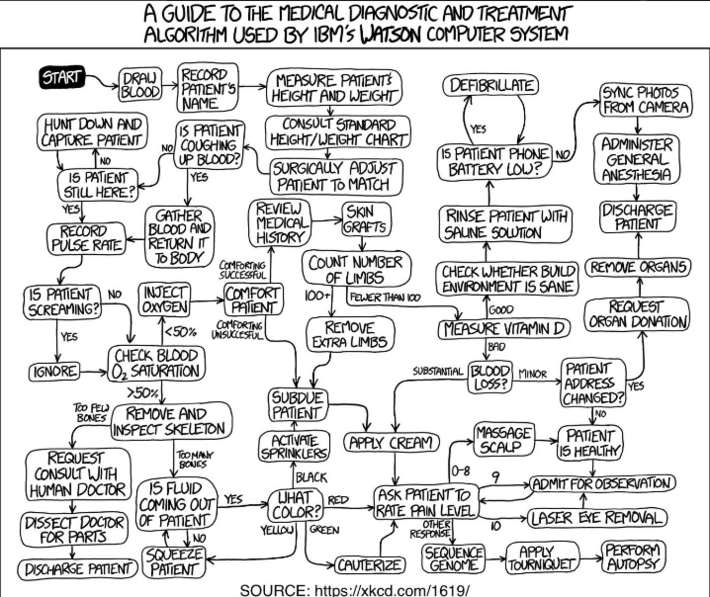
The common denominator among non-physician providers seems to be a high level of confidence they can provide medical care as well, and often better than, physicians. Is this confidence merited? Perhaps, in some situations; certainly not all. Time will tell. Unfortunately, patients, which includes everyone of us, will be the guinea pigs in this massive medical experiment. It behooves us to appreciate and consider the DunningKruger Effect.
https://www.bosshardtandmarzek.com/blog/confidence-is-overrated-the-dunningkruger-effect.html